During the first week of life, approximately 60% of term babies and 85% of premature infants develop jaundice [1].
Despite the pronounced symptoms, jaundice in most cases is not a serious threat and goes away on its own after two to three weeks.
But there are certain conditions under which jaundice must be treated to avoid serious complications. And the most effective and common form of jaundice treatment is phototherapy.
Here we take a closer look at the disease itself and the necessary nuances of treatment.
Causes of jaundice and when to treat it
Jaundice of newborns (hyperbilirubinemia) occurs when the child’s liver fails to cope with the breakdown of red blood cells, resulting in the accumulation of a byproduct — bilirubin. This is because the baby’s liver is taking over this job for the first time; before birth, the placenta and the mother’s liver perform this function.
Bilirubin gives the child’s eyes and skin a yellowish tint. Therefore, jaundice is easy to recognize by external signs.

Factors that may aggravate jaundice
As mentioned above, jaundice is a common occurrence in newborns that goes away on its own. But there are factors that can aggravate jaundice in a baby and turn it into a condition that requires treatment.
Factors that can exacerbate physiological jaundice in a baby include:
- Prematurity
- Hematoma
- Cephalohematoma
- Polycythemia
Polycythemia occurs when a child has more red blood cells than usual. It is the opposite of anemia, which is caused by a lack of red blood cells. - Delayed passage of meconium
Delayed passage of meconium, defined as a newborn’s inability to excrete it within 24-48 hours, is an important symptom in newborns and requires evaluation for disorders that lead to intestinal obstruction in newborns. - Breastfeeding
- Certain ethnic groups, especially the Chinese
Degrees of jaundice
All infants should be examined continuously in the first 4 days of life, especially those who are at risk of developing hyperbilirubinemia in the neonatal period.
In the first 48 hours of life, examinations should be performed at least 8-12 hours [2].
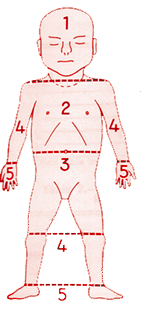
Jaundice usually starts at the head and spreads caudally to the trunk and extremities. This fact is used to tentatively estimate the level of jaundice by Kramer’s rule. Kramer divided the infant into 5 zones, defining an SBR range for each zone [3].
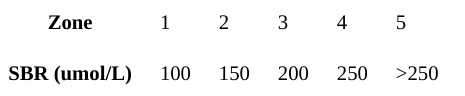
However, visual assessment of bilirubin levels can lead to errors, so there must be a low threshold for measuring serum bilirubin.
There are different degrees of jaundice, and the duration of the disease varies accordingly.
Despite the pronounced symptoms, jaundice in most cases is not a serious threat and goes away on its own in two to three weeks without medical intervention, says Billy Lou Short, M.D., chief of neonatology at Children’s National Center in Washington, D.C. In such cases, the doctor usually recommends more frequent feedings (every 2 to 3 hours) until jaundice passes, because this helps the baby process the excess bilirubin through more frequent defecation.

But if jaundice lasts too long, is accompanied by other factors, or if the child has risk factors such as premature birth, treatment is necessary [source: National Institutes of Health]. Because high bilirubin levels, if untreated, can cause brain damage (nuclear jaundice), leading to cerebral palsy, auditory neuropathy, visual impairment, and dental enamel hypoplasia.
If the jaundice lasts too long, is accompanied by other factors, or if the baby has risk factors such as premature birth, treatment is necessary.
The most effective and common form of treatment for jaundice is phototherapy. This treatment is used for several days until the liver is mature enough to process bilirubin on its own. Below, we take a closer look at all the nuances of this procedure.
Phototherapy for jaundice
A form of light therapy (phototherapy) that helps prevent complications in newborns with jaundice is called — bili lights.
The wavelength of light used, the intensity of the light source, the total light dose received (phototherapy time and amount of skin exposed), and/or the threshold at which phototherapy begins can affect the effectiveness of phototherapy in treating jaundice [4].
Usually, infants have to stay in the hospital for the entire period of treatment. Hospitals use special phototherapy machines, using regular or fiber-optic lights. It’s like babies are in some kind of weird blue tanning bed.
But thanks to new technology using bili blankets (also called jaundice vests), which have the right spectrum of light, therapy can also be done at home. However, this is only possible if the bilirubin level is moderate and there is no risk of diseases such as G6PD or Rh infection.
A bili blanket is used either in place of or in addition to a bili blanket. The blanket is a fiber-optic pad that is placed against the child’s skin, allowing the skin to directly absorb light. It is especially convenient for home use.

The phototherapy process
Protect the infant’s eyes
During bili light therapy, the infant’s eyes should be covered to prevent the retina from drying out and becoming irritated by the bright light. Soft protective goggles are worn by the infant. Otherwise, phototherapy is safe and causes no pain or discomfort to the child.
Ensure maximum access of light to the skin
Phototherapy involves illuminating the bare skin with fluorescent light. The light must hit as much of the infant’s skin as possible, so infants undergoing this treatment are not wrapped in blankets, placed under the light without clothes, or simply with a diaper, and nurses regularly turn the infant over to expose different parts of the body.
Monitor the condition
The medical team carefully notes the infant’s temperature, vital signs, and response to light. They also note how long the treatment lasted and the position of the bulbs. With home treatment, parents need to monitor the temperature themselves.
Take blood tests
During phototherapy, regular blood tests are taken (usually with a small sample taken from the child’s heel). This is done to determine the bilirubin level, and when it drops enough, you can stop the phototherapy. If phototherapy is done at home, a nurse comes daily and takes a blood sample for analysis.
Bilirubin levels will be checked every 4-6 hours after the start of phototherapy to see if the treatment is working. Once the child’s bilirubin levels stabilize or begin to drop, they will be checked every 6-12 hours.
Possible Risks
The most common risk associated with bili light therapy is dehydration, due to increased peripheral blood flow and diarrhea (if present). In such cases, infants sometimes receive fluids intravenously.
Other potential complications:
- Overheating — monitor the newborn’s temperature
- Diarrhea due to intestinal hypermobility
- Ileus (in premature infants)
- Rash
- Retinal damage if poor eye protection during the procedure
- Temporary lactose intolerance
- Grey-brown discoloration of the skin and mucus membrane (rare)
Duration of treatment
The duration of the phototherapy treatment varies from child to child, as each child’s condition is individual. Bilirubin treatment usually takes 24 to 48 hours, after which the newborn’s liver can handle the bilirubin on its own.
Newborns receiving phototherapy (in the absence of other contraindications) may have short periods (30 minutes every 3-4 hours) when phototherapy is stopped so that they can be cradled/breastfed and have their eyelids removed for parent-child interaction.
If the child’s jaundice does not improve after conventional phototherapy, continuous multiple phototherapy may be offered. This involves the simultaneous use of several light sources and often a fiberoptic coating.
The treatment does not stop during continuous multiple phototherapy. In this case, milk decanted from the mother’s breast in advance can be injected through a probe into the child’s stomach or through one of its veins (intravenously).
Documentation in the neonates’discharge letter and Child Health Booklet should include details about TSB/SBR levels and duration of phototherapy treatment.
Alternatives to phototherapy
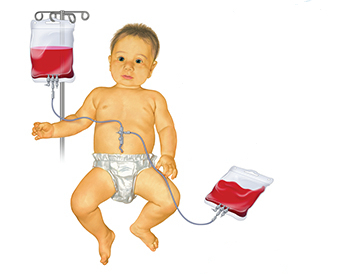
If neonatal jaundice requires treatment, phototherapy is usually used as a first-line clinical treatment. But if phototherapy does not work or in severe cases of elevated bilirubin in low birth weight infants who are less than 24 hours old, an exchange blood transfusion may be performed instead of phototherapy.
With this transfusion, the infant’s blood is slowly drained and replaced with donor blood or plasma, as this physically removes the bilirubin. But your baby must be in the ICU for this treatment, so it is not the first step.
Immunoglobulin transfusions are also possible, but this also requires a stay in the ICU. In extremely rare cases, surgery or medication is needed.
Adults with jaundice
Jaundice is not only found in infants. Adults get jaundice, too. Jaundice in adults can be caused by a variety of conditions, from viruses to genetic disorders to disease and trauma.
Bili light is not usually used to treat jaundice in adults. In newborns, jaundice is usually a temporary condition, so the biliary tracts just have to do their job until the infant’s liver functions are working.
In adults, jaundice is usually caused by a liver problem (such as hepatitis) or bile duct obstruction, gallstones, gallbladder or pancreatic cancer, and alcoholic liver disease.
Viruses such as Epstein-Barr (which causes mononucleosis) and medications such as paracetamol, birth control pills, and steroids can also cause jaundice.
Consequently, treatment of jaundice in adults requires diagnosis and treatment of the underlying cause. There is no specific treatment for jaundice in adults, the doctor will determine the underlying cause of the disease and focus on treating the condition.
Summary
Despite its symptoms, jaundice is not a serious threat in most cases and goes away on its own in two to three weeks without medical intervention. But if jaundice lasts too long, is accompanied by other factors, or if the baby has risk factors such as premature birth, treatment is necessary.
Treatment usually consists of phototherapy or, in rare cases, exchange blood transfusions.
There are 2 main types of phototherapy:
- Conventional phototherapy — when your baby is placed under a halogen or fluorescent lamp with his or her eyes closed
- Fiber Optic Phototherapy — when your child lies on a blanket with fiber optic cables; light passes through the fiber optic cables and hits your child’s back.
In both phototherapy methods, the goal is to expose your child’s skin to as much light as possible.
Usually, bili light phototherapy is effective in reducing bilirubin levels, and nothing else is needed. If phototherapy does not work, an exchange blood transfusion may be given instead.
FAQ
🩺 Why is phototherapy considered effective for jaundice?
High bilirubin levels, if left untreated, can cause brain damage. During bilirubin therapy, fluorescent or LED lights emit light that breaks down bilirubin into a form that the body can get rid of with urine and feces.
📍When should phototherapy be used for jaundice?
Despite the pronounced symptoms, jaundice in most cases is not a serious threat and goes away on its own after two to three weeks, but if jaundice lasts too long, is accompanied by other factors or if the baby has risk factors such as premature birth, treatment is necessary.
💡 What kind of light is used to treat jaundice?
Phototherapy uses light with wavelengths between 420 and 470 nanometers to break down bilirubin.
📅 What is the duration of biliary light treatment for jaundice?
The duration of phototherapy treatment differs individually, depending on each child’s condition. Treatment lasts until the problem is resolved, which is usually 24-48 hours, after which the newborn’s liver can deal with the bilirubin on its own.
⏳ How long do infants spend under bili light?
Newborns receiving phototherapy (in the absence of other contraindications) may have short periods (30 minutes every 3-4 hours) when phototherapy is stopped so that they can be held/breastfed and their eyelids removed for parent-child interaction.
🏠 Can baby jaundice be treated at home?
Thanks to technology using billy blankets (also called jaundice vests), which have the right spectrum of light, phototherapy can be done at home. However, this is only possible if the bilirubin level is moderate and there is no risk of diseases such as G6PD or rhesus infection.
Sources
- Subcommittee on hyperbilirubinaemia, American Academy of Pediatrics. Management of hyperbilirubinaemia in the newborn infant 35 or more weeks of gestation, Clinical Practice Guideline. Pediatrics 2004, 114(1): 297-316.
- NHS National Institute for Health and Clinical Excellence. Neonatal Jaundice: A Clinical Guideline.
- Kramer LI. Advancement of Dermal Icterus in the Jaundiced Newborn. Amer J Dis Child. 1969; 118: 454-458.
- Woodgate P, Jardine LA. Neonatal jaundice: phototherapy. BMJ Clin Evid. 2015 May 22;2015:0319. PMID: 25998618; PMCID: PMC4440981.
- Queensland Maternity and Neonatal Clinical Guideline Neonatal Jaundice: prevention, assessment, and management, Queensland Government (2009)
- Maisels MJ, McDonagh AF. Phototherapy for Neonatal Jaundice. N Engl J Med 2008; 358(9): 920-928.
- Lease M. Whalen B. Assessing jaundice in infants of 35-week gestation and greater. Current Opinion in Pediatrics 2010; 22: 352-65.