Phototherapy has been around for over 3000 years. Today, the use of this method in medicine is increasing and is becoming more and more popular for the treatment of various skin diseases, where local therapy is powerless.
One of the most effective phototherapy treatments is PUVA therapy. The team of our research institute decided to study and determine the features of PUVA therapy and its effect on the human body.
In this article, we have highlighted the main areas of application of PUVA therapy and considered the side effects. We also reviewed scientific studies and determined the effectiveness of this treatment method.
What is PUVA therapy and how it works
What is PUVA therapy?
PUVA, or psoralen plus ultraviolet A (UVA) radiation, is one of the oldest, most effective treatments for psoriasis. It is also known as photochemotherapy, as it combines the use of psoralen (a drug that makes the skin more sensitive to light), and exposure of skin to a source of high-intensity, long-wavelength, ultraviolet (UV) light.
Psoralens are natural chemicals substance in the seeds of various plants (legumes, parsley, figs). The psoralen molecule under the influence of UVA light can integrate into the DNA of bacteria, viruses, fungal, thereby damaging them and preventing reproduction.
Thus, if they are present in the skin at the time of exposure to UVA light, they greatly increase the effect of the light on the skin. This increased sensitivity is the key to the beneficial effect of PUVA treatment of skin disorders. It is important to emphasize that psoralens alone do not affect skin or skin disorders. In tandem with UVA light, this therapy is effective in treating a variety of skin conditions.
The psoralen most frequently used in PUVA treatment has the generic name of methoxsalen.
Ultraviolet light is divided into UVA, UVB, and UVC.
See the content
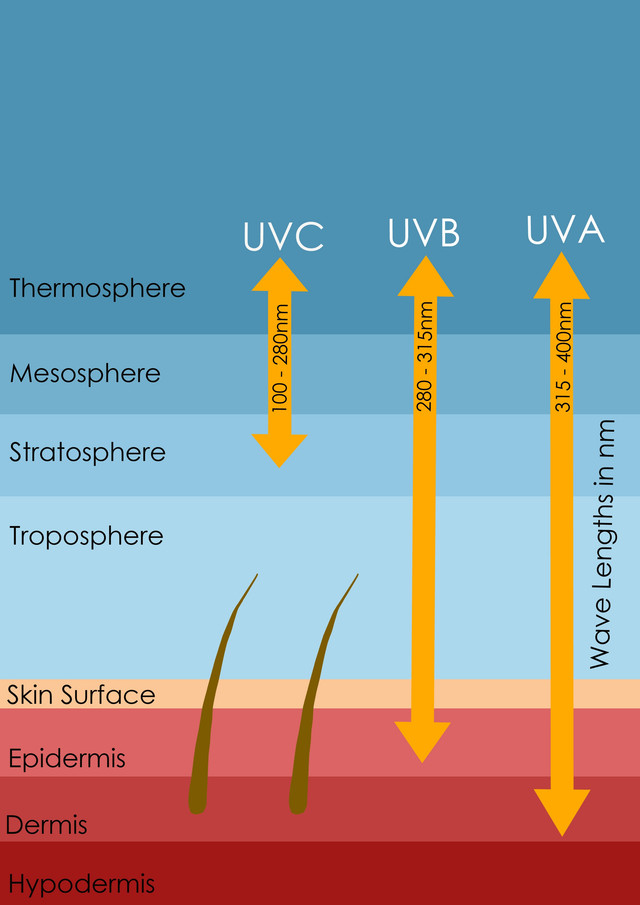
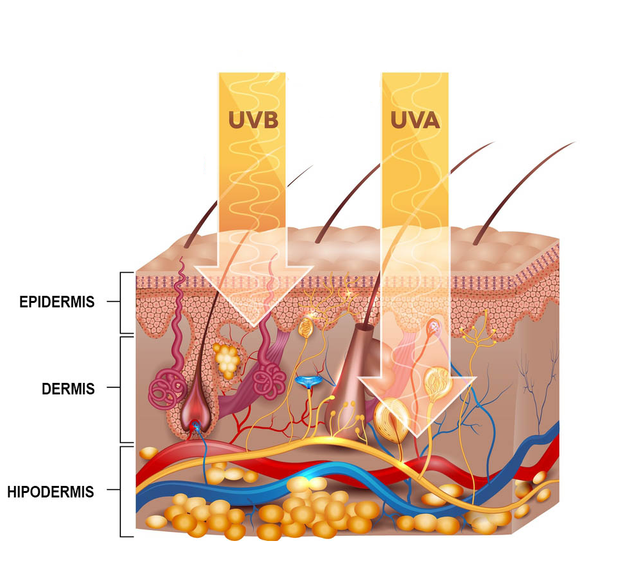
UVC light (100–280 nm) does not reach the surface of the earth since it is absorbed by ozone in the atmosphere. UVB light (280–315 nm) does reach the surface of the earth and this waveband is responsible for producing a sunburn and a suntan when we are exposed to sunlight. UVA light (315–400 nm) also reaches the surface of the earth and is composed of the longest wavelengths in the ultraviolet spectrum. Under normal natural conditions, UVA light from sunlight does not produce any significant short-term change in the skin. This type of wave is used for PUVA therapy.
How it works

There are three types of PUVA therapy: systemic PUVA (methoxsalen taken orally), hand and foot soak PUVA (methoxsalen dissolved in water for hand/foot soaking), and bath PUVA (methoxsalen dissolved in a bathtub for whole body soaking).
PUVA therapy involves the ingestion of psoralen and then exposure to UVA light one hour later. The dose of psoralen you take is held constant and is determined by your weight. The interval between taking psoralen and being exposed to light is also held constant because peak levels of psoralen in the skin are usually reached between one and two hours after ingestion [1].
The variable in the treatment is the dose of UVA light you are given. The initial dose is low and determined by either your past history of sunburning or by testing your response to PUVA. The dose of UVA light is gradually increased in subsequent treatment as your tolerance to the treatment increases [1].
The power of the treatment courses varies over time and different courses emit different amounts of UVA light. Therefore, even if your dose of UVA light is constant, the time for your treatment will vary from day to day. Treatment will be required 2-4 times each week until your skin disease has cleared [2].
What diseases does PUVA therapy treat?
PUVA photochemotherapy is a widely used light-based treatment for a range of diverse skin diseases and can be highly effective, well-tolerated, safe, cost-saving, and reduce the need for topical therapies [3].
PUVA therapy is beneficial in more than twenty different diseases and it acts via at least two different mechanisms:
1. Killing skin cells
Many skin diseases are caused by cells of the body’s immune system. They either multiply too quickly or behave abnormally, disrupting the life of the system. PUVA therapy destroys these cells without harm to our immunity. Psoriasis, eczema, lichen planus, alopecia, and mycosis fungoides are just a few of the diseases that are amenable to PUVA therapy.
2. Increased resistance to sunlight.
PUVA therapy enhances skin pigmentation and also increases the thickness of the epidermis. Both of these effects reduce sensitivity to sunlight. Thus, treatment with PUVA is beneficial for disorders characterized by hypersensitivity to sunlight, such as vitiligo, polymorphic light rash, and solar urticaria.
How effective is PUVA therapy? Based on scientific research

Psoriasis
Psoriasis is a skin condition that occurs when the immune system is imbalanced. Redness appears on the body, scaly plaques that are difficult to treat. It is believed that psoriasis develops due to genetic disorders. As a result of chronic inflammation, it develops not only in the skin but also in other organs and systems.
Most often, psoriasis occurs on the knees, elbows, and scalp. They can also appear on the palms, feet, back, and any other part of the body.
For about 40 years, PUVA therapy has been prescribed as a treatment for severe psoriasis. PUVA is often prescribed when the local use of drugs and UVB is ineffective.
In 2013, a randomized study [4] was conducted in which 74 patients with moderate to severe plaque psoriasis took part. Of the patients included in the study, 38 received the PUVA bath and 36 received the PUVA system. The study continued over a 6-week treatment and 4-week follow-up period. The aim was to compare PUVA bath and systemic PUVA therapy in the treatment of psoriasis.
The result was a significant reduction in the area of psoriasis in both cases. Within 6 weeks, PUVA bath therapy reduced the value by 74% (from 16.4 to 4.2), and systemic PUVA by 62% (from 15.3 to 5.8).
Below is an example of this study.
*Click or hover to unblur the image

Source: US National Library of Medicine, National Institutes of Health
Several studies [5] were conducted between 2003 and 2010, involving 172 patients with moderate to severe chronic plaque psoriasis. One-half of the patients received PUVA therapy, while the other half received topical treatment (biologics: adalimumab, alefacept, etanercept).
The result showed a decrease in the area of psoriasis by 86% with PUVA therapy, while treatment with drugs in the general population gave only 40% results.
From this, it can be concluded that the effectiveness of PUVA is superior to that of some biological products and is recommended for the treatment of moderate to severe psoriasis.
Eczema
Eczema is a chronic inflammatory skin condition that causes itching, redness, and rashes in the form of small blisters. This is a genetically determined disease. Eczema occurs quite often it is diagnosed in about 30-40% of patients visiting a dermatologist.
Although any light-based approach to treating eczema is less straightforward than psoriasis, not least because of the exacerbation of eczema in the early stages of treatment, PUVA can be a highly effective treatment.
In a study [6] participated 17 patients with chronic hand eczema were treated with topical PUVA for 8 weeks. As a result, significant improvement was achieved in 5 cases (29%), moderate improvement in 9 (53%), and a slight improvement in 3 (18%). Since topical PUVA has no risk of systemic side effects, it should be considered as an alternative treatment for patients with chronic hand eczema resistant to other topical drugs.
The resistance of the disease to traditional local treatment prompted another study [7], which involved 28 patients with chronic palmar or plantar eczema. Bath-PUVA therapy was carried out 4 times a week for up to 25 procedures. Excellent or good effects were achieved in 93% of patients with the palmar disease and 86% of patients with plantar eczema.
The results of the study are presented below.
*Click or hover to unblur the image
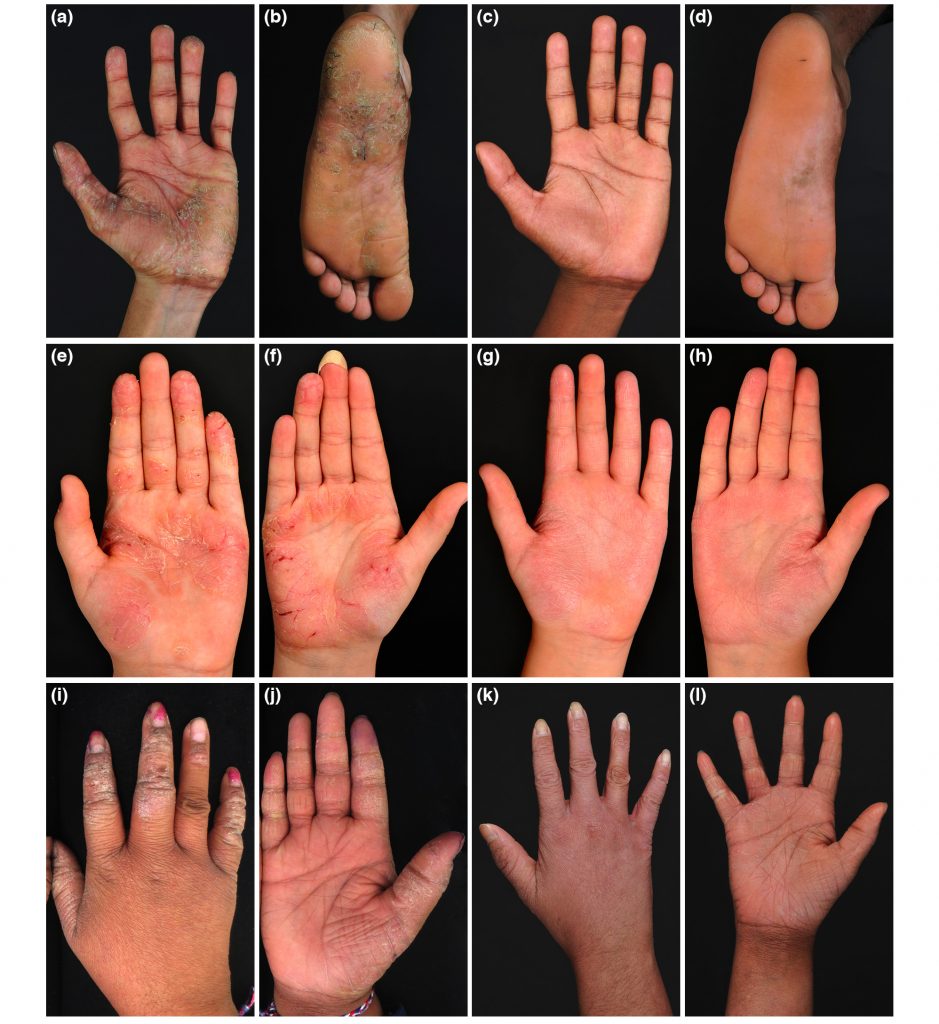
Source: US National Library of Medicine, National Institutes of Health
Thus, it can be concluded that the local bath-PUVA therapy is of great importance in the treatment of chronic palmar-plantar eczema, which is resistant to the standard methods of local treatment.
Mycosis fungoides
Mycosis fungoides is a skin disorder characterized by red spots, induration, and scaling of the skin; sometimes internal organs and lymph nodes are affected. Outwardly, these changes resemble skin fungus, hence the name “mycosis fungoides”. The disease progresses very slowly, over years or even decades.
Light therapy is an important treatment option for this disease, both in early-stage and advanced patients. Mycosis fungoides, like other hematological diseases, are extremely radiosensitive, so treatment with low doses can provide a high response rate [8].
In 2012-2018, a study [9] involving 27 patients with mycosis fungoides at an early stage received PUVA therapy. As a result, this treatment caused high rates up to the complete disappearance of the foci of the disease in 19 patients, which is 70% of those fully recovered. And the subsequent maintenance phase of PUVA prolonged remission without signs of disease. During treatment, no adverse reactions of the body to PUVA therapy were observed.
The result of the treatment is presented below.
*Click or hover to unblur the image
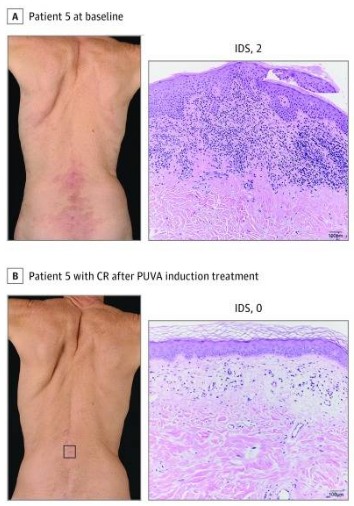
Source: US National Library of Medicine, National Institutes of Health
This study demonstrates that PUVA therapy provides a highly effective treatment for the early stages of mycosis fungoides.
Vitiligo
Vitiligo is a disease characterized by the disappearance of from the skin. It can negatively influence the physical appearance of affected individuals, and may profoundly affect a person’s psychosocial function and quality of life [10].
Treatments for vitiligo are generally unsatisfactory as there are no methods that lead to a complete repigmentation, although there are many methods that cause a partial response. PUVA therapy has been used as the main treatment modality for patients with vitiligo.
Between 1985 and 1997, a study [11] was conducted on 33 patients with vitiligo. They received systemic PUVA therapy, which resulted in a positive response to treatment. In half of the patients, repigmentation was 51–75%, and in six patients, repigmentation was more than 75%. It should be noted that lesions on the face and trunk showed better repigmentation than other areas (hands, feet).
Also, from 1990 to 2001, a study [12] was conducted in Saudi Arabia, which included 32 patients with vitiligo. The overall response rate to treatment was 59.4%. As mentioned in an earlier study, the hands and feet were the most resistant sites to treatment.
*Click or hover to unblur the image

Source: US National Library of Medicine, National Institutes of Health
Thus, it can be concluded that PUVA is considered the most appropriate and effective treatment for vitiligo. But before starting PUVA therapy, it is necessary to take into account the distribution of vitiligo-skin integuments, since the response to treatment varies greatly depending on the area of the body.
Effectiveness of PUVA Photochemotherapy vs NB-UVB Phototherapy
Ultraviolet (UV) light therapy is one of the most widely used treatments for skin conditions. Phototherapy is typically used when skin involvement is widespread and/or topical treatments have proven to be ineffective or impractical.
UVA and UVB are wavelengths of light found in natural sunlight and are used for phototherapy. NB-UVB phototherapy includes broadband ultraviolet B (290-320nm) and narrowband ultraviolet B (311nm), while Psoralen with UVA has 320-400nm wavelengths. In general, UVB reaches the more superficial skin layer of the epidermis, while UVA penetrates deeper into the dermis.
We reviewed scientific studies of the most common skin conditions that used PUVA and NB-UVB phototherapy to compare treatment efficacy.
Psoriasis
The main indication for any light therapy is psoriasis, and for the reasons stated in terms of the practicality and ease of treatment, as well as its safety and potential for use in children and pregnancy, NB-UVB phototherapy usually comes first [13].
A comparative study [14] was carried out in which 10 patients with psoriasis. As a result, no significant differences in efficacy were seen between twice-weekly NB-UVB or systemic PUVA. However, there was a trend towards higher efficacy of PUVA for patients with a higher baseline score, suggesting a role for PUVA in more severe psoriasis or recurrent psoriasis.
Also, in a separate study [15], 100 patients with psoriasis received twice-weekly PUVA therapy, which was superior to twice-weekly NB-UVB. That said, 35% of patients were still being clear 6 months after completing PUVA, compared to only 12% after NB-UVB. These results are supported by the results of a study in which 93 patients with chronic plaque psoriasis were randomly assigned to receive either twice-weekly PUVA therapy or twice-weekly NB-UVB. This resulted in 84% achievement of PUVA removal of psoriasis compared to significantly lower removal rates with NB-UVB (65%).
Thus, as a conclusion from this study findings, NB-UVB should usually be considered as the first phototherapeutic option for patients with light form psoriasis. PUVA therapy used for chronic plaque psoriasis, when NB-UVB is not effective or there is rapid relapse once NB-UVB is discontinued [13].
For children, NB-UVB phototherapy is preferred and PUVA is relatively contraindicated, although this is not an absolute rule. But given the concerns about long-term safety, PUVA would not be the first-line choice.
Eczema
A small randomized study [16] was conducted, where 12 patients with severe atopic eczema. Half of the patients were treated with bath-PUVA and the other with narrow-band UVB radiation.
All showed marked improvement or complete remission with both treatment regimens. The mean baseline decreased by 65.7% with the PUVA bath and 64.1% with the narrow-band UVB treatment. No serious adverse reactions were observed with either of the two regimens.
Consequently, the data confirm the high efficacy of PUVA baths and narrow-band UV-B phototherapy in the treatment of patients with severe atopic eczema.
It can be concluded that NB-UVB phototherapy and PUVA photochemotherapy are effective treatments for skin diseases. They should be given priority not only for psoriasis but also for various other inflammatory diseases, including eczema and mycosis fungoides. The treatment is well tolerated with few side effects. Based on the research results, it is worth noting that the role of PUVA is more effective in severe or recurrent skin diseases. Since entry-level, NB-UVB is the preferred approach due to its greater usability.
Nevertheless, choosing a method of treatment should be guided by the conclusion of the attending physician and susceptibility to light waves.
Side effects and risks caused by PUVA therapy
The side effects of PUVA therapy can be divided into short-term and long-term.
Short-term side effects:
- Erythema (redness)
An overdose of PUVA can lead to a sunburn-like reaction. This is more likely in fair-skinned patients who tan easily. Therefore, it is recommended to avoid exposure to sunlight throughout the day from the time of taking psoralen. To minimize this reaction, it is advised to wear clothing that covers the entire body.
Unfortunately, erythema can last longer than sunburn from natural sunlight. Moisturizers and pain relievers can reduce discomfort.
- Itching
PUVA therapy dries out the skin and this can cause itching. This is usually corrected by the regular use of emollients.
- Nausea
When psoralen is taken orally before exposure to UVA-light, some patients may experience nausea. In this case, it is recommended to eat a snack containing a little fat (for example, cheese, nuts) after taking the medicine.
Long-term side effects:
- Freckles
Exposure to PUVA therapy in light susceptible individuals may cause freckles. They usually disappear after stopping treatment, but subsequent exposure to sunlight will usually reactivate them.
- Eye damage
If the eyes are not protected from UV radiation, damage can occur that results in red, painful eyes. Another possible risk is damage to the lens of the eye, leading to cataracts.
This potential problem can be completely avoided by using suitable eye protection during therapy.
- Skin cancer
Long-term exposure to PUVA therapy can lead to the same type of skin cancer caused by chronic exposure to sunlight. People with fair skin or those who have been previously affected by the sun or radiation are at the greatest risk. This is not a concern for most patients who receive PUVA therapy for only two to three months.
Patients who receive long-term maintenance PUVA therapy should undergo a skin examination by a specialist at least once every 6 months. It is advised to pay the doctor’s attention to any new moles and slow-healing wounds.
Summary
PUVA therapy is one of the most popular treatments for skin diseases such as psoriasis, eczema, vitiligo, fungal mycosis when local therapy is powerless.
Treatment with PUVA therapy consists of taking psoralen and exposing the skin to UVA light. This procedure has no serious side effects if you follow the precautions. But it is worth considering that after a session of light therapy, there may be short-term effects such as itching, redness. The skin becomes more sensitive to light under the influence of psoralen, so the treatment takes some time to recover.
FAQ
⏳ How long do I need to wait before I start seeing results after PUVA therapy?
The duration of treatment depends on the disease and the patient’s predisposition to PUVA therapy. Usually, patients with psoriasis and eczema see the first result after a few weeks, which is much faster than patients with vitiligo (several months).
⌚ How long does the effect of PUVA therapy last?
Most skin conditions, such as psoriasis or eczema, cannot be completely cured by any remedy. However, after treatment with PUVA therapy, a large number of patients find that their condition remains satisfactory for several months, and often much longer.
💵 How much does PUVA treatment cost?
The price of PUVA therapy depends on the number and duration of sessions. For an adult, treatment usually costs about $4,000-5,000 per year.
🏠 Can I do PUVA therapy at home?
PUVA therapy is traditionally used in hospitals and related facilities, but it can also be done at home if the necessary equipment is available and safety standards are met. A doctor’s prescription is required to purchase.
Sources
- Schneider LA, Hinrichs R, Scharffetter-Kochanek K. Phototherapy and photochemotherapy. Clin Dermatol. 2008;26(5) – p.464–476. doi: 10.1016/j.clindermatol.2007.11.004.
- Melski JW, Tanenbaum L, Parrish JA, Fitzpatrick TB, Bleich HL. Oral methoxsalen photochemotherapy for the treatment of psoriasis: a cooperative clinical trial. J Invest Dermatol. 1977;68(6) – p.328–335. doi: 10.1111/1523-1747.ep12496022.
- Norris P, Hawk J, Baker C, Bilsland D, Diffey B, Farr PM, et al. . British Photodermatology Group guidelines for PUVA. Br J Dermatol. (1994) 130:246–55. 10.1111/j.1365-2133.1994.tb02910.x
- M Berneburg, T Herzinger, J Rampf, W Hoetzenecker, E Guenova, C Meisner, J Maetzke, T Schaefer, B Eberlein, K Scharffetter-Kochanek, M Rocken. Efficacy of bath psoralen plus ultraviolet A (PUVA) vs. system PUVA in psoriasis: a prospective, open, randomized, multicentre study. – Br J Dermatol. 2013 Sep;169(3):704-8. doi: 10.1111/bjd.12466.
- Martin Inzinger. Efficacy of psoralen plus ultraviolet A therapy vs. biologics in moderate to severe chronic plaque psoriasis: Retrospective data analysis of a patient registry. May 2011British Journal of Dermatology 165(3):640-5 DOI: 10.1111/j.1365-2133.2011.10396.x
- Gritiyarangsan P, Sukhum A, Tresukosol P, Kullavanijaya P. Topical PUVA therapy for chronic hand eczema. Clinical Trial J Dermatol – 1998 May;25(5):299-301. doi: 10.1111/j.1346-8138.1998.tb02401.x.
- Schempp C, Muller H, Czech W, Schopf E, Simon J. Treatment of chronic palmoplantar eczema with local bath-PUVA therapy. J Am Acad Dermatol – 1997 May;36(5 Pt 1):733-7. doi: 10.1016/s0190-9622(97)80326-x.
- Trowell O.A. The sensitivity of lymphocytes to ionizing radiation. J Pathol Bacteriol. 1952;64:687–704
- Pablo Vieyra-Garcia, Regina Fink-Puches, Stefanie Porkert, Roland Lang. Evaluation of Low-Dose, Low-Frequency Oral Psoralen–UV-A Treatment With or Without Maintenance on Early-Stage Mycosis Fungoides. JAMA Dermatol. 2019 May; 155(5): 538–547. doi: 10.1001/JAMA Dermatol.2018.5905
- Ongenae K, Beelaert L, van Geel N, et al. Psychosocial effects of vitiligo. J Eur Acad Dermatol Venereol 2006;20(1):1–8.
- Sahin S, Hindioğlu U, Karaduman A. PUVA treatment of vitiligo: a retrospective study of Turkish patients. Int J Dermatol – 1999 Jul;38(7):542-5. doi: 10.1046/j.1365-4362.1999.00654.x.
- Tallab T, Joharji H, Bahamdan K, Karkashan E, Mourad M, Ibrahim K. Response of vitiligo to PUVA therapy in Saudi patients. Int J Dermatol – 2005 Jul;44(7):556-8. doi: 10.1111/j.1365-4632.2004.02014.x.
- Archier E, Devaux S, Castela E, Gallini A, Aubin F, Le Maitre M, et al. . Efficacy of psoralen UV-A therapy vs. narrowband UV-B therapy in chronic plaque psoriasis: a systematic literature





Is it safe to use PUVA therapy in the treatment of scalp psoriasis?
How long can treatment with PUVA therapy cause skin cancer? Are there such patients?
How to eliminate itching and redness after treatment with PUVA therapy? And is it possible to avoid these consequences?